What is Epilepsy
Epilepsy is a disorder of brain that leads to recurring seizures. These seizures can present in various forms, ranging from dramatic events like severe body shaking accompanied by loss of consciousness, as seen in generalized tonic-clonic seizures, to brief episodes that resemble daydreaming.
These various types of seizures are broadly classified into partial/ focal seizures and Generalised seizures.
What causes Epilepsy?
Seizures occur due to sudden and excessive electrical discharges in the brain, disrupting normal functioning. In focal/ partial epilepsy, it starts from one part of brain and known as “focus” of epilepsy and in generalised epilepsy, excessive electrical discharges start/ almost instantly spread to whole brain. The cause of epilepsy can vary widely and includes genetic factors, brain injuries, infections, and developmental disorders.
How is epilepsy diagnosed?
Epilepsy is primarily diagnosed by doctors, neurologists, or epilepsy specialists, relying heavily on the accounts provided by patients and eyewitnesses. The sensations experienced prior to the events, referred to as an aura, along with a thorough eyewitness description, play a crucial role in the diagnosis of epilepsy.
Additionally, diagnostic tests such as electroencephalograms (EEGs) are often employed to detect abnormal electrical activity in the brain, which can help confirm the presence of epileptic seizures. Brain imaging tests like MRI or CT scans are used to identify any structural abnormalities in the brain that cause this condition.
Role of Brain scan/ Neuroimaging in Epilepsy
Brain scans, such as CT scans or MRIs, are performed to identify the underlying cause of epilepsy. Typically, doctors recommend these scans, except in a few specific types of epilepsy, such as absence epilepsy, juvenile myoclonic epilepsy, or benign Rolandic epilepsy.
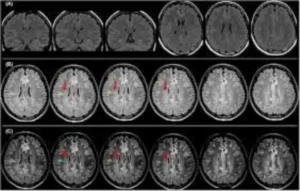
These imaging techniques help in identifying any structural abnormalities, such as tumors, lesions, infections like Neurocysticercosis, areas of brain damage, that might be contributing to the seizures. By providing detailed images of the brain, these scans enable healthcare professionals to make more accurate diagnoses and develop effective treatment plans.
These scan results are crucial for understanding the effectiveness of anti-seizure medications. Specific findings, such as Mesial temporal sclerosis and Dysplasia, are linked to a less favourable response to standard medical treatments and epilepsy surgery can be very effective.
Type of Brain Scans in Epilepsy
- Structural brain imaging like CT scans and MRI
- Functional imaging like PET scan, SPECT and fMRI
- Multimodality scans
Each tests have different indication to be done. Functional and multimodality imaging are reserved for difficult to treat epilepsy or medically refractory epilepsy.
MRI vs CT scan of Brain
A specialized epilepsy protocol MRI of the brain is the preferred investigative method in epilepsy. In contrast, a CT scan has a very limited role and provides significantly less information than an MRI.
How is Epilepsy protocol MRI different from routine MRI of Brain?
An epilepsy protocol MRI includes additional studies (Known as sequences) of Brain that maximize the chance of detecting lesion/ abnormality in brain that produces seizures. It specially focusses on areas of brain that are often responsible for seizures.
Temporal lobe epilepsy is commonest cause of refractory epilepsy; hence, these scans are designed for detail study of this area and specially look for hippocampus volume, signal changes and distortion of architecture. Presence of these features is termed as Hippocampal sclerosis or mesial temporal sclerosis.
An epilepsy protocol MRI involves supplementary studies, that enhance the likelihood of identifying lesions or abnormalities in the brain that cause seizures. This approach particularly targets regions of the brain frequently associated with seizure activity.
Temporal lobe epilepsy is the most common cause of refractory epilepsy; therefore, these scans are specifically tailored for an in-depth examination of this area, with a focus on the hippocampus’s volume, signal changes, and any architectural distortions. The presence of these characteristics is known as Hippocampal sclerosis or mesial temporal sclerosis.
A skilled radiology team can identify abnormalities that may lead to frequent seizures, even when only minor changes are present in a small area of the brain. These subtle issues may be overlooked if the MRI study is not specifically targeted. Radiologists must be informed about the potential brain region where the neurologist suspects the seizures originate.
Do we need to give contrast injection for MRI in Epilepsy?
No. A limited number of patients need contrast study, usually when a neurologist requests it due to specific clinical characteristics or previous imaging results. Also, if there is some abnormality detected in epilepsy protocol study where radiologist feels giving contrast will help to understand problem better.
I have Calustrophobia. I feel suffocated inside MRI machine. I am afraid of undergoing MRI due to loud sound. Is there a comfortable way for me to undergo MRI?
MRI scans are safe and come with outstanding safety features. While the sounds can be somewhat bothersome, Catalyst’s MRI scanner boasts a wider tunnel to enhance your sense of security. Headphones are provided, and the technologist plays soothing music of your choice to ease your anxiety. Our team is trained to help calm you and address your concerns. Most patients find that their fears were unfounded and that the procedure was, in fact, quite pleasant.
There is a special mode for reduced noise scanning that can be utilized for individuals who find sound intolerable. While this mode may take a few extra minutes compared to the standard setting, the quality of the images remains uncompromised.
However, a small percentage of patients with moderate to severe claustrophobia may struggle to overcome their fear, even with standard approaches like counseling, education, and familiarization with the MRI system and process. While an open MRI can be an alternative, its image quality is generally inferior to that of a closed MRI system. Some patients may find relief through relaxation techniques like deep breathing exercises or guided meditation prior to their appointment. In certain situations, a mild sedative may be prescribed to alleviate acute anxiety, ensuring the patient can undergo the necessary imaging with the least discomfort possible. By tailoring the approach to the individual needs of each patient, healthcare professionals can help ensure that even those with significant claustrophobia can access the diagnostic benefits of MRI technology.
For some patients, open MRI can be considered speciality where loss of some details is not expected to change the management. However, if patient has refractory epilepsy, a high-quality epilepsy protocol MRI may be must and short sedation/ day care anaesthesia may have to be considered as last resort.
Ultimately, the goal is to create a comfortable and supportive environment that prioritizes the patient’s mental and emotional well-being, ensuring that their experience with MRI technology is as positive and stress-free as possible.
Do advanced functional imaging like PET and SPECT scan are needed for all patients?
These scans are designated exclusively for a specific group of patients, making up less than 5% of the total epilepsy population. This primarily includes rare epilepsy syndromes, cases of medically refractory epilepsy where MRI and VEEG fail to yield sufficient information, and individuals seeking certain advanced treatments.